Breastfeeding
Helpful information and resources for when you are breastfeeding.
Need help now?
Call the Australian Breastfeeding Helpline:
Ph: 1800 Mum 2 Mum
Ph: 1800 686 268
The South East Sydney Local Health District also runs Breastfeeding Support Groups.
For further resources, visit breastfeeding.asn.au or refer to the relevant sections below.
Helpful Breastfeeding Videos
Breastfeeding in the First Week
Tips to help you and your baby as you learn to breastfeed.
Building Milk Supply
Many women worry that they will not have enough breastmilk for their baby. Many women stop breastfeeding because they feel like they don’t have enough milk. If a mother’s breastfeeding is genuinely low it is usually only a temporary situation.
Common reasons why women perceive their milk supply is low:
Baby feeds too often: It is natural for a baby to feed frequently (8-12 times per day). Baby can be unsettled but it does not mean that there is not enough milk. Frequent feeding is necessary to establish a good supply.
Breasts feel soft: As your supply adjusts to what your baby’s needs are, your breasts will not feel as full but as long and your baby continues to feed well your breast will make sufficient milk
Baby starts feeding frequently all of a sudden: This usually happens when your baby goes through a “growth spurt”. This increased frequency in feeding will help to increase your supply as your baby grows.
Possible causes of low supply:
- Poor attachment or sucking
- Baby not feeding often enough - the more milk removed from the breast the more milk is produced
- Waiting until your baby is crying before you feed will lead to the baby not feeding well - it is best to offer the breast when the baby starts to stir
- Using formula - will reduce demand therefore reducing your supply
- Breast reduction or surgery
- Large amounts of alcohol, nicotine and caffeine
- Recently had mastitis and can cause a sudden drop in supply
- Physical reasons- a small number of women may not have enough glandular tissue to produce enough milk for their baby
- Some medications can affect breastfeeding - discuss all medications prescribed and over the counter with your doctor or pharmacist to evaluate their effect on your supply.
How to increase milk supply:
- Regular skin to skin at the breast
- Ensure your baby is attached well and has unrestricted access to the breast
- Feed frequently at least 8-12 times
- Express by hand or pump after a breastfeed to remove more milk so the breast will produce more
- Change sides several times during a feed especially if your baby is sleepy - this will stimulate them to suck strongly and trigger more let-downs
- Offer your breast as a comforter for a few days instead of a dummy
- Avoid stress - rest when you can and maintain a good diet
- Avoid giving other foods
- Medication to increase supply - discuss this with your healthcare provider
Remember Supply = Demand
Healthy Eating for Breastfeeding Mothers
Caffeine and Breastfeeding
Too much coffee can lead to your baby becoming:
- Unhappy
- Jittery
- Colicky
- Sleeps poorly
Recommendations
- The Food Standards Australia and New Zealand recommends up to 200mg caffeine can be safely consumed
- Only 1% of the amount of caffeine enters your breastmilk - the level of caffeine in your breastmilk reaches it peak amount 60 minutes after you drink it
- Caffeine can make nipple vasospasm and nipple sensitive worse in some women
- Smoking will increase the effects of caffeine on your baby.
Caffeine quantities in food and beverages
Drink | Caffeine content |
Espresso Coffee | 145mg/50ml shot |
Takeaway Coffee | 51-332mg/serve |
Instant Coffee (1tsp/cup) | 60-80mg/250ml cup |
Tea – Black, Green and Matcha (most herbal teas have no caffeine) | 10-50mg/220ml cup |
Milk Chocolate | 20mg/100g |
Dark Chocolate | 43mg/100g |
White Chocolate | 0mg |
“Energy” Drinks or Formulated caffeinated drinks | Up to 80mg/250ml can |
Coca Cola | Up to 54mg/375ml can |
Alcohol and Breastfeeding
The National Health and Medical Research Council recommendation is “for women who are breastfeeding, not drinking alcohol is safest for the baby”.
- Alcohol is in your breast milk 30-60 minutes after you start drinking.
- Generally every standard drink takes 2 hours to be clear from your breast milk
- The concentration of alcohol in your blood and breast milk is the same
- There are a few steps to help make drinking alcohol during breastfeeding the safest possible
- Download FeedSafe App from the Australian Breastfeeding Association to help calculate your drinks
- General rule
- is to always breastfeed your baby before you drink and eat before and while you are drinking
- Consider planning ahead by expressing in advance to have breast milk available in case you are unable to feed your baby or if necessary formula may need to be used if it there is no safe breast milk available
- No amount of pumping and dumping will clear alcohol from your breast milk any faster. Once your bloodstream is clear of alcohol your will also be clear.
- Arrange for someone who is not affect by alcohol to care for your baby where possible and do not sleep with your baby
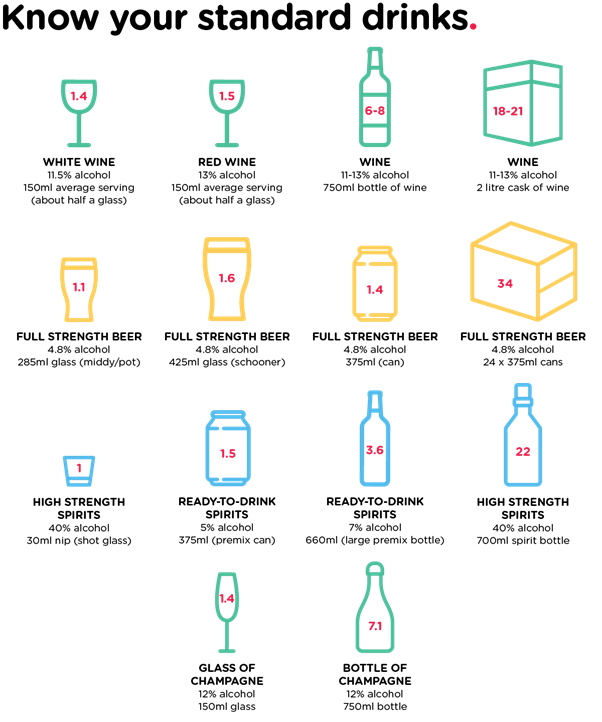
What is a standard drink?
- 100ml of 13.5% wine
- 1 ‘stubby’ (375ml) of mid-strength beer
- 1 pre-mixed bottle (275ml) (alcoholic seltzers 5%)
- 30ml of spirits
Common Myth:
- Alcohol is good for your milk supply - in fact alcohol stops breast milk from flowing freely.
Engorgement
Many women’s breasts become engorged when their milk comes in. It is not just the amount of milk that increases but also an increase in blood supply. Your breasts may feel large, tight and very uncomfortable which can make it difficult for your baby to attach well to the breast.
Ways to relieve engorgement:
- Feed your baby frequently: Feeding often is the best way to prevent your breasts from getting too full. If your breasts become full and uncomfortable you may need to wake your baby to feed or express enough for comfort.
- Take your bra off completely before starting to breastfeed: Babies feed better when they have free access to the breast. When your breasts are very full, feeding without a bra will be more comfortable.
- Wear a supportive bra after feeds that is not too tight
- Apply warm compresses before feeds
- Massage your breast to encourage a let down
- Massage or use breast compressions on the breast while feeding
- If a baby feeds from only one side you can express the other breast just enough for comfort.
- Express a little before feeds if your baby has trouble latching and staying on: Full, tight breasts may flatten the nipple therefore hand expressing a little to soften the areola (area around the nipple) to help your baby attach more easily.
- Use pain relief as required
- Use cold packs (bags of frozen peas work well as they shape around the breast or frozen nappies)
- Reverse pressure softening can be used to soften overfull breasts before feeding or expressing.
- Washed cold, green cabbage leaves can provide relief (not red as it will stain and is too soft):
- NOTE: DON’T USE cabbage if you are allergic to sulfur
- Remove any hard stems from the leaves - the leaves can be crushed to help mould to the breast.
- Cover the breast with the leaves. Leave the nipple exposed (covering nipples may cause them to become too moist and if there are any cracks. Cabbage should not be used) Leave them on until they wilt, which is usually 20-30 minutes.
- Wear a bra or tank top to hold them in place. You can reapply fresh leaves for up to one hour of continuous application. For 3-4 times a day.
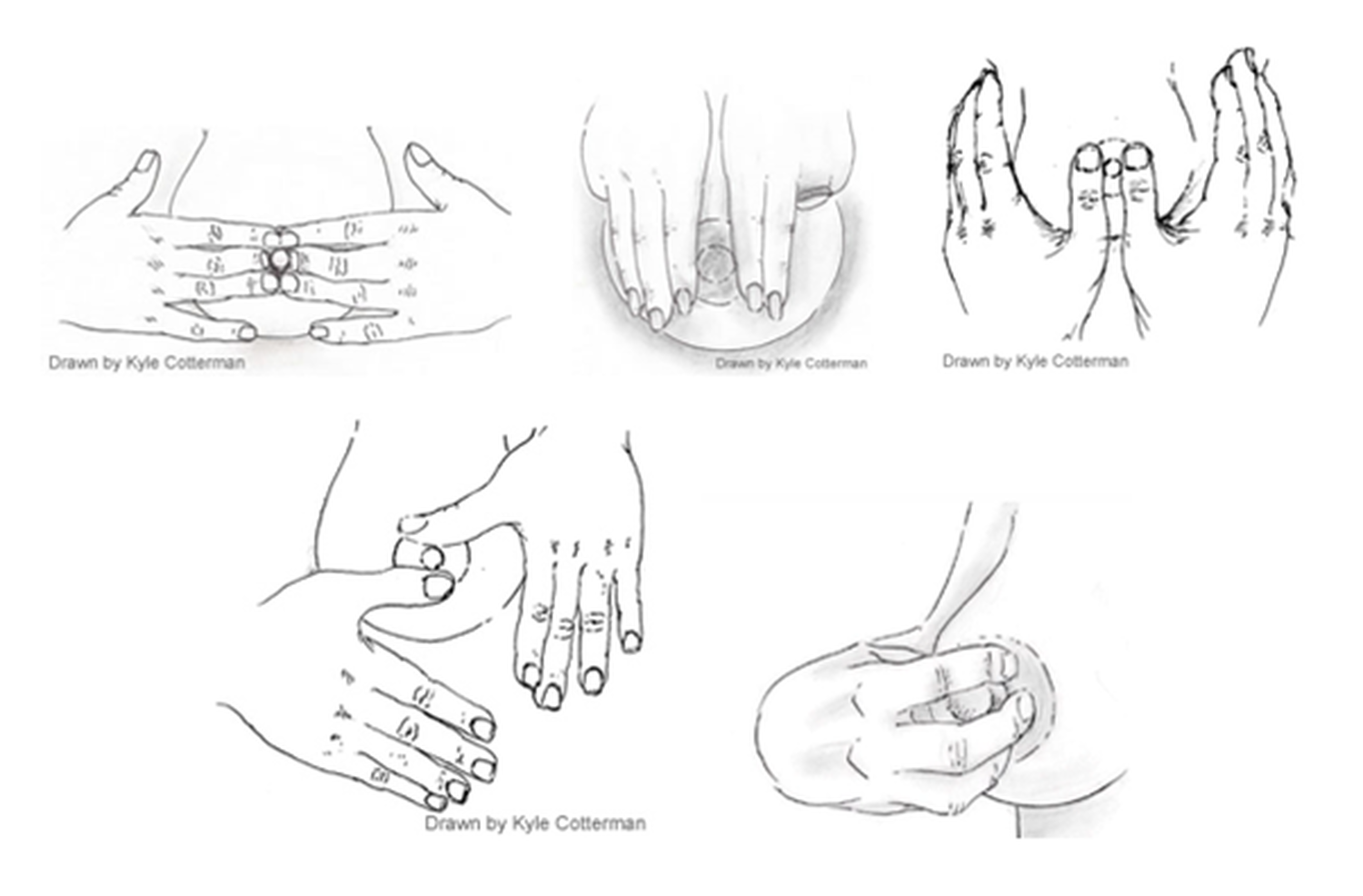
Reverse Pressure Softening
Reverse pressure softening is a strategy to assist with latching when a mother is engorged. Reverse pressure softening is to soften the areola and temporarily move some of the swelling slightly backwards and upwards into the breast. The firmer the areola the more time is required to soften.
Steps to Reverse Pressure Softening
- Press your fingertips around the base of your nipple (any finger combination may be used)
- Firmly but gently, apply steady pressure (not causing pain)
- After 30 seconds or so, drag your fingers away from your nipple, continuing to apply pressure.
- Continue the same process alternating positions around your nipple
- Repeat until your areola has softened
- Latch your baby or express milk right away
Oversupply/Too Much Milk
Some mothers make more milk than their baby can cope with.
Signs of an oversupply
- Breast seem to fill very quickly
- The breasts are often lumpy and tight, despite softening with a breastfeed
- Baby gags and gulps especially at the begin of a feed and only wants to feed on one breast
- Baby may bring up a lot of milk after a feed
- Baby gains a lot of weight quickly
- Increased fussiness between breastfeeds
- Lots of wet nappies more than the 5-6 normal nappies
- Watery explosive and often green bowel motions at each feed.
Managing an oversupply
- Breastfeed from one breast only at each feed - allow your baby to feed for as long as they need - if the other breast feels full, then hand express enough for comfort.
- Block feeding - this involves offering the same breast for a set period of time such as 3 hours
- Every time the baby wants to feed during this 3 hour period they are to feed on the same breast
- If the second breast becomes uncomfortable during this time express enough for comfort
- Do the same on the other breast
- Once supply has settled the mother and baby can return to normal demand feeding.
- Feeding in a different position can help
- Positions such as leaning back cradle hold or football, laid back position and lying down can reduce the fast flow and allow baby to feed without gagging
- If the mother is comfortable she can try and place her baby in a sitting/upright position to feed
- Only express for comfort or to help baby latch deeply if your breast is too full or hard
- Limit comfort sucking at breast by using soothing techniques such as rocking or a dummy
- Use cold packs between feeds to make your breast feel more comfortable
- Burp baby every 3-4 minis and then put back to same side to finish feeding
- Feed frequently therefore less milk accumulates between breastfeeds
- Express by hand or pump until the first let down and the put the baby on the breast.
Breastfeeding with Large Breasts
Mastitis
Understanding Mastitis, what to do and when to contact your GP.
Nipple Shields
Download the Medela Nipple Shield sizing guide below.

